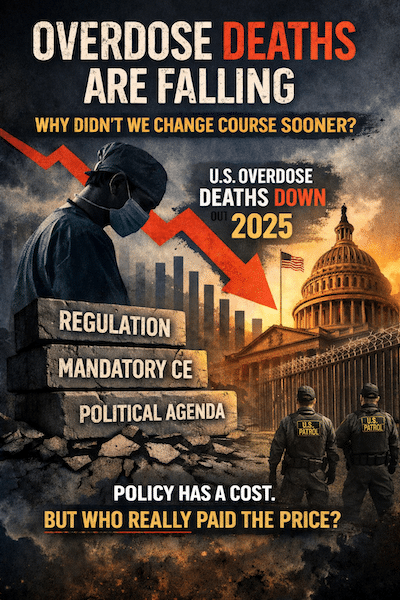
And it raises an uncomfortable question:
If progress is possible now, why was it politically impossible before?
Policy Is Not Neutral. Elections Have Consequences.
For years, the dominant narrative was simple and convenient:
Clinicians prescribe. Patients overdose. Regulators intervene.
That story justified:
- sweeping regulatory expansion,
- punitive oversight of healthcare professionals,
- and an explosion of mandatory “education” programs with questionable impact.
But the data never fully supported that narrative.
Now, overdose deaths are falling—without further constricting legitimate clinical care. The implication is unavoidable:
The crisis was never as simple as policymakers claimed.
And simplicity was never the goal. Control was.
Who Actually Paid the Price?
While policymakers debated optics, clinicians absorbed the consequences.
Dentists, physicians, and surgeons were:
- recast as risk vectors,
- subjected to escalating compliance burdens,
- forced into performative CE rituals that often had more to do with liability shielding than patient outcomes.
Meanwhile, the overdose epidemic continued—largely driven by illicit synthetic opioids, not clinical prescribing.
If deaths can decline meaningfully without further criminalizing healthcare, then the past decade of policy deserves re-examination—not celebration.
The Education Industrial Complex
Mandatory opioid CE was sold as a moral imperative.
But ask honestly:
- Did it meaningfully reduce overdose deaths?
- Or did it primarily create a compliance economy?
- Who benefited—patients, or institutions?
When outcomes improve only after political winds shift, it becomes harder to pretend that prior policies were purely evidence-based.
They weren’t.
They were ideological.
Clinicians Were Never the Core Problem
Clinicians matter—but not in the way regulators suggested.
Dentists do not run addiction treatment programs.
Physicians do not control illicit fentanyl markets.
Surgeons do not manufacture xylazine.
Yet clinicians were treated as if they did.
Why?
Because clinicians are visible, regulated, and politically safe targets.
Drug cartels are not.
A Dangerous Pattern
Here is the deeper issue:
When policy is driven by symbolism rather than evidence, healthcare becomes a stage prop in political theater.
And when elections change, the script changes.
The tragedy is that patients and clinicians live with the consequences long after the slogans fade.
The Dojo Position
We support:
- rational prescribing,
- legitimate education,
- and evidence-based risk mitigation.
We do not support:
- performative regulation,
- scapegoating of clinicians,
- or the rewriting of history when outcomes finally improve.
If overdose deaths are falling, that is good news.
But good news should trigger accountability, not amnesia.
Because in healthcare—just like in politics—
elections have consequences.